80 YR OLD MALE WITH COUGJ AND DIFFICULTY IN BREATHING.
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
80p year old male with cough and difficulty in breathing since 2 years
An 80 year old male patient, farmer by occupation, resident of Nalgonda came to the hospital with
CHIEF COMPLAINTS of cough and difficulty in breathing since 2 years, which aggravated since 2 months
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 2 years ago then he had complaints of shortness of breath which was insidious on onset and gradually progressive .
No associated wheeze
No orthopnea
No seasonal variations, no pnd
No history of recurrent upper/ lower respiratory tract infections
Also complaints of cough since 2 years
Associated with sputum, copious in amount, mucopurulent, yellowish colour, foul smelling
Not associated with blood
Cough aggravated on lying down
No seasonal variations
No chest pain, palpitations, syncopal attacks
PAST HISTORY
K/C/O TB 30 years back, used medication for 4 months
K/C/O HTN since 5 months
N/K/C/O DM, CAD, Asthma , epilepsy
PERSONAL HISTORY
Diet mixed
Appetite Normal
Bowel and bladder movements regular
Sleep adequate
Addictions Alcohol and smoking which was stopped 40 year ago
GENERAL EXAMINATION :
Patient is c/c/c , moderately built and nourished
No pallor, icterus, cyanosis ,clubbing, lymphadenopathy, pedal edema
Vitals:
Temp- afebrile
PR- 78bpm
BP- 110/70 mmhg
RR- 18cpm
SpO2- 97% at RA
SYSTEMATIC EXAMINATION
RESPIRATORY SYSTEM EXAMINATION
Oral cavity- hard palate , soft palate, uvula , tonsils , posterior pharyngeal wall - normal
Dental caries present.
URT
Nose - No septal deviation or Nasal polyps
LRT
1.INSPECTION
Shape of the chest - elliptical
There is drooping of shoulder towards left side
Trachea appears to be central
Equal movement of chest wall on both sides
No usage of accessory muscles
No scars ,sinuses ,engorged veins, edema
2.PALPATION
No local rise of temperature , no tenderness
Trachea deviated towards the left side
Movement of chest wall - slightly decreased on left side
AP diameter is 22cm and Transverse diameter is 28 cm
Chest circumference -
On inspiration- 86.cm
On expiration - 86cm
Tactile fremitus - right left
Supraclavicular normal increased
Infraclavicular normal increased
Mammary normal increased
Axillary normal increased
Infra axillary normal increased
Suprascapular normal increased
Infrascapular normal increased
Interscapular normal increased
Vocal resonance -
Right left
Supraclavicular Normal increased
Infraclavicular Normal increased
Mammary Normal increased
Axillary Normal increased
Infraaxillary Normal increased
Suprascapular Normal increased
Infrascapular Normal increased
Interscapular Normal increased
3. PERCUSSION
Right left
Direct Normal decreased
Supraclavicular Normal decreased
Infraclavicular Normal decreased
Mammary Normal decreased
Axillary Normal decreased
Infra axillary Normal decreased
Suprascapular Normal decreased
Infrascapular Normal decreased
Interscapular Normal decreased
INVESTIGATIONS
Chest x- ray
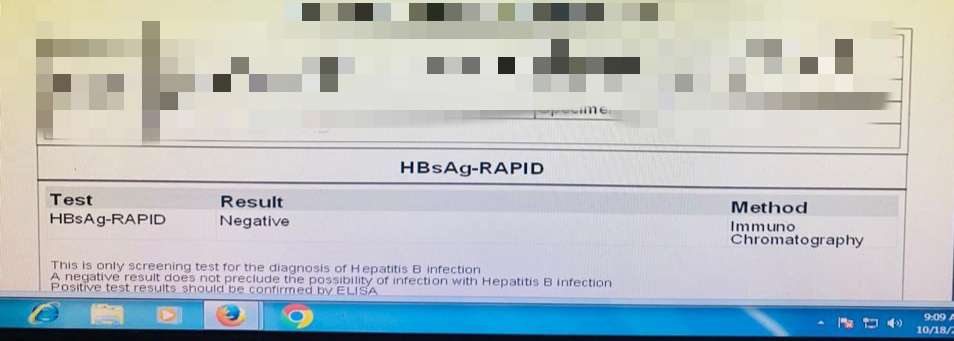
Serological tests
LFT
SERUM ELECTROLYTE
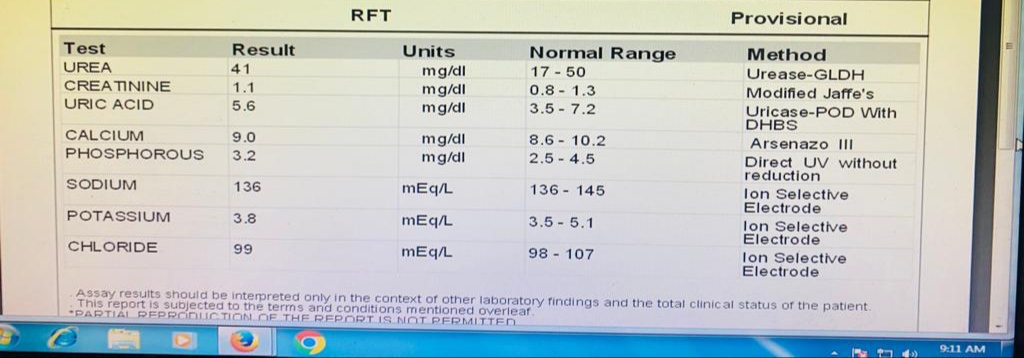
RFT
Provisional diagnosis:
LEFT COLLAPSE OF LUNG
k/c/o BRONCHIAL ASTHMA
k/c/o HYPERTENSION
Treatment:
17/10/2023
-Inhaler formoterol and budesonide 2 puffs/ SOS
-T. TELMA 40 mg PO/OD
-syp.ASCORIL -LS 10 ml/ PO/ TID
18/10/2023
-Inhaler formoterol and budesonide 2 puffs/ SOS
-T. TELMA 40 mg PO/OD
-syp.ASCORIL -LS 10 ml/ PO/ TID
-Neb. with BUDESONIDE 12th hourly IPRAVENT 6th hrsly
19/10/2023
-Inhaler formoterol and budesonide 2 puffs/ SOS
-T. TELMA 40 mg PO/OD
-syp.ASCORIL -LS 10 ml/ PO/ TID
-Neb. with BUDESONIDE 12th hourly IPRAVENT 4th hrsly